So, what’s the plan?
The vast majority of people over 50 say it’s important that they keep living in their current homes for as long as possible. But a new poll shows many of them haven’t planned or prepared for “aging in place,” and a sizable percentage might have a hard time paying for in-home help.
The pandemic’s toll on older adults, especially those in nursing homes and other long-term care facilities, has brought the issue of living independently at home into the national spotlight. So have policy proposals around changing the ability of Medicare and Medicaid to pay for virtual care and in-home help.But the new findings from the National Poll on Healthy Aging suggest many people in their 50s, 60s, and 70s need to do more to modify their homes or plan for services they may need if they want to avoid or delay needing to move. The poll also shows differences in aging-in-place readiness among the 28 percent of older adults who told the poll that they live alone.
The poll is based at the U-M Institute for Healthcare Policy and Innovation (IHPI) and supported by AARP and Michigan Medicine, the University of Michigan’s academic medical center.
Consider this
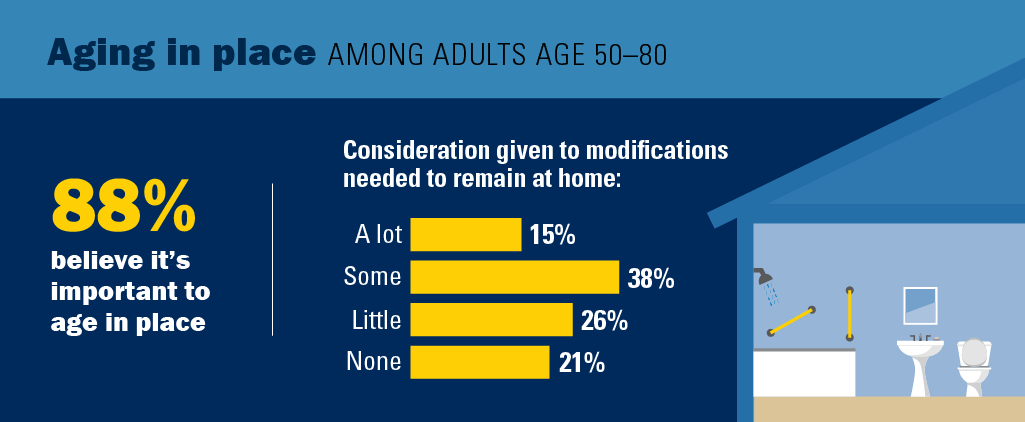
In all, 88 percent of people between the ages of 50 and 80 said it was very or somewhat important to them that they live in their homes as long as possible. But only 15 percent said they’ve given a lot of consideration to how their home may need to be modified as they age, while 47 percent have given it little or no thought.
Meanwhile, 48 percent of those who live alone said they don’t have someone in their lives who could help them with personal care such as bathing and dressing if needed, compared with 27 percent of those who live with others.
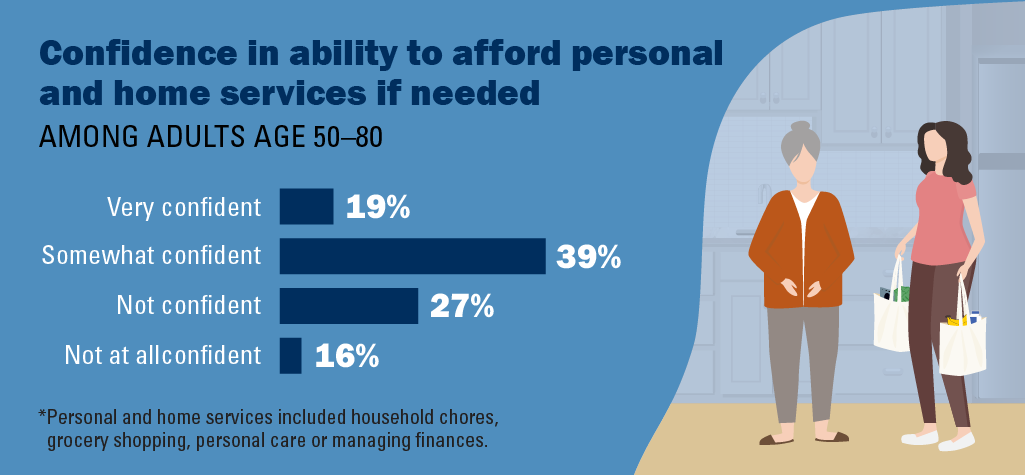
As for hiring help, 19 percent of older adults are very confident they could afford to pay someone to help with household chores, grocery shopping, personal care, or managing their finances.
On the other hand, nearly two-thirds of those who called their current physical or mental health status fair or poor said they were not confident or not very confident that they could afford to pay for such help.
“The pandemic’s impact on older adults, and policy proposals about home-based services at the federal and state level, mean this is a topic of immediate importance,” said Sheria Robinson-Lane, PhD, MHA, MS, RN, an assistant professor at the U-M School of Nursing and IHPI member who worked with the poll team on the report. “Especially for those without as much social support, or with more health needs, it’s important to take a proactive approach and plan for the future now.”Poll director Preeti Malani, MD, a U-M Medical School infectious disease professor also trained in geriatrics, said that older adults should explore with their health care providers and local social service agencies the kinds of support available to them, and talk with loved ones about their goals.
“Taking steps to understand what’s available in the community, through the national Eldercare Locator, the Area Agency on Aging that serves your region, nonprofit organizations, and other sources could help older adults be more prepared,” she said. “Family members can help encourage older adults to find out what’s available, to invest in home improvements, and to aid them in installing safety devices and technologies that can help keep them aging in place. Think of it as a positive investment toward current safety and future independence – that can help older adults get past the temptation to put it off for another day.”
More findings
The poll finds that one in five older adults had moved in the past five years. About half of those who moved said they had moved to a home that was easier to get around, while half also said their new home was smaller.Wherever they live now, 34 percent said their home definitely has the necessary features that would let them age in place, and 49 percent said they had at least one ‘smart home’ device.
But the poll drilled down to ask about specific features and technologies. While 88 percent had a main-floor bathroom and 78 percent had a bedroom on the main floor, which could reduce the need to climb stairs and reduce fall risk, fewer older adults had other features.
For instance, 32 percent said they had grab bars in the bathroom, and less than 10 percent had safety-focused technologies such as alarms on their stoves or personal emergency response systems. Only 7 percent said they had a barrier-free shower, and 9 percent said that it was difficult to use the main rooms in their home because of clutter or large amount of possessions there.
“AARP research consistently shows that the majority of older adults want to stay in their homes and communities for as long as possible,” said Indira Venkat, VP of consumer insights at AARP. “Unfortunately, most houses weren’t built to support the needs of people across the many stages of life. The best way to continue living in the home you love is to plan ahead and make changes that will accommodate your needs today and in the future.”
In late 2021, AARP published a report on the preferences of adults over 18 about their future home and community circumstances, including the ability to age in place.
The poll report is based on findings from a nationally representative survey conducted by NORC at the University of Chicago for IHPI, and administered online and via phone in January and February 2022 among 2,277 older adults age 50-80. The sample was subsequently weighted to reflect the U.S. population.
Read past National Poll on Healthy Aging reports and about the poll methodology.
Read more about this topic and other medical news at the blogs Michigan Health and Michigan Health Lab.




Ken Powell - 1973
I have no concern whatsoever about aging in my home. Know why? I’ll move when I need to. Places under consideration are waterfront home, lakefront home, beach home and space.
Reply
Beth Friel - 1983
“I’ll know when I need to move” is not always true. My mother in law said the same thing. She lost the right to drive after crashing through the iron gate to her community and totaling her car. Still, she was not ready to move. She got progressively worse dementia and could not write checks or make meals. Still not ready to move. She set the stove on fire when she forgot she was cooking something. Still not ready to move. We found her on the floor, unconscious, lying in her waste and vomit. Still not ready to move. Finally, she was so weak she could not get out of bed. We had to call an ambulance and she arrived at the ER with a UTI and sepsis. She survived but could not be released home. We finally moved her into assisted living after a tremendous toll on friends and family. Long term care decisions are not just about the individual. Family members are not often able to take on all the care responsibilities and the emotional toll is horrendous. My husband and I are making detailed plans so we don’t put our children through what our mothers have put us through. “I’ll know when it is time” is an unkind act of denial.
Reply
Todd Stuart - 1985
Not every senior is in denial about their needs and capabilities. My parents faced tremendous pressure (nagging) to move into senior housing and/or assisted living, which would’ve meant downsizing their living space, selling most of their possessions, disrupting and losing control over their lives and facing the expense of senior housing.
They chose instead to modify their home and hire help. Later my mother passed away after a short hospital stay; my father a month later during hospice at home. Staying at home was manageable and better for them.
Reply
Debbie Rech - 1992
Beth, this is so powerful and such a painful story to read. I’m so sorry you experienced this trauma over and over again. The emotional toll is horrendous and it is such an unkind and selfish act of denial. Thank you for sharing. I’m saving it for future conversations.
Reply
Beverly Trebesch - MSW 1986
I’m fortunate my mother and I reside together. We’re healthy, we exercise and laugh daily. Plus,she enjoys
watching University of Michigan sports on television. We are lucky. I’m hoping to read more in-depth research-based articles about older individuals. Go Blue — everyday, every way, everywhere to everyone !
Reply
Debbie Rech - 1992
Aging in place and with dementia is a real problem in the US. The challenges reach way beyond money and grab bar, although both help tremendously. The quality of home health aides in this country is at an all time low. I haven’t done a comprehensive study but I saw firsthand what it’s like in south Florida, home to a dense population of our elders. I was a live in companion for an 87 year old homebound but mobile woman with dementia. She has five adult children and only one lives locally with his family. They rarely visited which meant my presence bought them safety and freedom while her fluctuating dementia became my imprisonment. It took a toll on my mental health. The part time home aides who relieved me twice a week so I could enjoy time away from the house were a joke. They were basically house sitters who dispensed meds and served meals that I prepared. The home health agency we hired told me that their industry was decimated by the pandemic and many aides sought less demanding employment and better wages, paid time off, health care, etc. Fact is our elderly need us to help them live their best final chapters. But how do we do that with prohibitive costs and inadequate caretakers? Aging in place is a wonderful idea in concept but then it also creates social isolation. The television becomes the companion and that is so not good. We need more senior living colonies like Burbank Senior Artist Colony where the residents engage one another on a daily basis. This is living. The woman I cared for for eight months was ultimately moved into an assisted living facility end of March. She is angry, resentful, confused, and suffering. What a horrible way to exist. We’ve got to do better. And to everyone reading this wondering if I’m available to take care of your loved one and/or Kara, if you’d like to chat in depth about what I learned being on the frontlines of elder care and dementia, yes to both. We’ve got to change the model of aging in America. We’re too smart and we’ve got untapped resources. We can do better. We owe it to ourselves, our parents, and generations trailing us.
Reply
Lynn Stephenson - 1979
Debbie touched on my worst fear. Quality of care. My husband and I have moved to a smaller lakeside home. One story living with a walk in shower in the master. Quiet community but with good healthcare. Grocery and pharmacy deliveries no issue. Lots to do to stay active and engaged. We both even have very good long term care insurance. I would say we’re much better prepared than most. Unfortunately, that doesn’t guard us against poor quality in those we have come to our house for care in our later years. I saw first hand the huge range of abilities and levels of empathy in those that cared for my father in his home as he aged. That is one thing none of us have control over, and must find a way to insure.
Reply
Debbie Rech - 1992
Lynn, please feel free to connect with me off of this thread for peace of mind. I’d be glad to hop on a phone call with you so we can begin a conversation. In the event that you or your husband need care and I’m available, I’m always glad to be there for a fellow Wolverine. This article and the conversation are obviously bringing to light all the holes in elder care that truly need to be addressed. Since working with my Miami Beach client, I’ve been routinely reaching out to multiple aging in place and dementia/Alzheimer’s foundations, organizations and institutions. Response rate is low unfortunately. It’s great that billions of dollars are being spent to research dementia and Alzheimer’s but equal attention and funds need to be directed to the now – to the salaries and paid time off for non family caregivers working 12-24 hour days/shifts without protection by employment law, to the salaries for family caregivers who either give up their careers, take time off or work after hours. As you can see, I’m lit up by this discussion. I’ll continue to use my passion, my compassion, my voice and these Michigan platforms to make a difference.
Reply
Sushil Birla - 1997
This article addresses a growing societal problem. Whereas this article reported the study on elder readiness for aging in place, we need additional study and focus on the systemic societal issues identified by Debbie Rech and Lynn Stephenson. (I hope Dr. Preeti Malani sees this). The infrastructure is neither supporting good eldercare in nursing homes nor in senior living communities nor in own homes. In the communal care setting, long-term insurance becomes practically useful only when one has lost self-care capability for the long term. It does not help when one is declining gradually and needs care by others intermittently. We hired (at our own expense) homecare aides when my wife returned home after spinal surgery. Our experience matches what Debbie and Lynn reported.
The physical facilities (e.g.: grab bars; shower chairs; toilet seats; decluttered spaces) for aging in place are not the issue. Even in multi-level homes, one can manage through the use of chair lifts.
Reply
John Knight - 1913, 1919
We just purchased a home, our long-term tomb, in a 55 and older Desert community, complete with a clubhouse, activities, etc. The house has no stairs, easy in and out bathrooms, and excellent weather. We will die here. With all this said, we have no one. It’s just us. I hope that we can sustain our lifestyle without draining our 401k’s, relying solely on Medicare, or panhandling. I often think about reaching out to organizations highlighted in this article. However, in the end, I say to myself, “I’ll do it tomorrow.” My wife and I are in excellent health. We don’t plan on getting a dreaded disease like dementia. But who does? My advice to everyone is to take this article seriously. Don’t wait until tomorrow!
Reply
Debbie Rech - 1992
John, please feel free to connect with me off of this thread for peace of mind. I’d be glad to hop on a phone call with you so we can begin a conversation. In the event that you or your wife need care and I’m available, I’m always glad to be there for a fellow Wolverine. This article and the conversation are obviously bringing to light all the holes in elder care that truly need to be addressed. Since working with my Miami Beach client, I’ve been routinely reaching out to multiple aging in place and dementia/Alzheimer’s foundations, organizations and institutions. Response rate is low unfortunately. It’s great that billions of dollars are being spent to research dementia and Alzheimer’s but equal attention and funds need to be directed to the now – to the salaries and paid time off for non family caregivers working 12-24 hour days/shifts without protection by employment law, to the salaries for family caregivers who either give up their careers, take time off or work after hours. As you can see, I’m lit up by this discussion. I’ll continue to use my passion, my compassion, my voice and these Michigan platforms to make a difference.
Reply
Jaqueline Farber - 1997
The way the elderly are treated in this country is deplorable. People are forced to have less than $2,000 in assets in order to qualify for placement in a long term care facility. Many elderly folks (or anyone who is unfortunate to be hospitalized with a long term illness) must spend all of their savings, sell their homes, cars and everything else they have worked for their entire lives in order to spend their final days in a understaffed, poorly run facility. Also known as Nursing Homes.
Doctors contribute to this by giving false hope to terminal patients who have no hope of a decent long-term quality of life, “this surgery will give you the best chance at recovering from your stage 4 terminal inoperable cancer” while the outcome as often as not ends up with the patient spending their final days, weeks, months, hospitalized; intubated and suffering. The same patient could have been counseled by a palliative care team prior to acute illness and may have made the decision to die at home with family and friends.
None of us has adequately prepared for our inevitable demise(s). This failure is in no small part due to our healthcare system being solely focused on making money. They intentionally seek to profit off of the illnesses, the misery and the suffering of our family members, friends and neighbors.
It could all be so much better.
Reply
Jackie Armstrong - 1974, 1978
We will all die, The fear that grips some commentators is not in my heart. Our children have clear instructions to let us hold onto our independence and dignity even as safety risks increase. We may fall, forget meds, eat less than nutritionally optimal meals, even wander off in a blizzard. At the end of the day, the end is inevitable and a part of the great circle of life. No Bingo games for me, let me choose to end my days while living my life as I choose. I am not persuaded that a longer life in a confinement facility is a fitting finale.
Reply
Free Polazzo - 1967
Everyone is already “aging in their place”.
Reply
Shirley Tepper LaMere - 1957
yep. look at that date! I am 86, my husband 84. Before he came home from the re-hab for a broken hip, I had made all the additional adjustments needed in our one story home. But in-home care is VERY expensive; I suspect more-so in California where we live. I get less able all the time and now have a cleaning lady once a week, who will also grocery shop, but have to face the problem of what to do next. Do not want to hire an in-home helper every day until that is really necessary. We have the savings, that isn’t the problem, it’s HOW to use them best. It is a scary prospect but we are more than ever determined to make it work.
Reply
Christopher Burke - 1975 (HS), 1979 (BFA), 1982 (MS from UM)
After seeing our elderly mothers decline when they reached their late 80s and early 90s, we spent the last two years designing a major renovation to our home to allow us to age in place. The plans check the all the boxes for ADA/elderly living compliance.
Our financial planner assured us that we could afford the hefty mortgage that this project would require without compromising our retirement plans. We are both in our early to mid 60s and anticipate full retirement in three years.
The problem? Projected construction costs have escalated well past the amount that we mortgaged—making us question if we are about to do the right thing (construction has not started yet).
My wife, who has always questioned if this was a good idea, now wants to kill the project. She would prefer to downsize; I would rather stay in our house of 30+ years.
We are struggling about what to do. Should we go for it—knowing the costs could creep up even higher? Or kill the project and see what we will really need as our years advance? (I have challenged my wife to come up with a better alternative to where we are now, but she has not come up with a convincing “Plan B”).
It is causing a great deal of stress. We are each adamant about our respective views, but we also have our respective doubts: “what if I’m wrong and the other person is right?”
How do we navigate our way through this?
Reply
Debbie Rech - 1992
Christopher, Sounds like you’ll both be right. How can either of you be wrong when you’re both coming from a place of love and looking out for each other and your finances? Looking it the situation in absolutes is what feels wrong. You have to remove the blame game from this or else you’re entering the ‘final’ decision with a cloud hanging over you. Saying ‘I told you so’ literally works zero percent of the time. Bottom line is you both want to feel safe in whatever route you go and you want to feel comfortable. Maybe map out the current costs of downsizing versus modifying and tour a few downsized options. You might find yourself pleasantly surprised at the options. Or, you could both see that the downsized options aren’t aligned with the picture of your future. Also, keep in mind that part of that picture might include a bedroom/bathroom for any overnight home health care aide(s) you may need in the far future.
Reply
Christopher Burke - 1982
Hi Debbie:
Thank you for your insight. We looked at small sample of downsize options. The trade offs in terms of location and amenities don’t touch we would have if we renovate. (I know; I want to have my cake and eat it too).
You make an interesting point about in-house arrangements if any overnight care is ever required. A care giver can be easily accommodated if we stay where we are. The same can be said if one of us contracts a debilitating illness and the healthy spouse cannot stay in the same bedroom for whatever reason. Much easier to do with where we already are…
Reply
David Lawrence - 1965 B of Architecture
I am retired from the practice of architecture, which essentially a concept of working with a client, to solve a problem they believe is in the building realm.
17 years ago my wife and I moved into a new condominium (at the time). She recently passed suddenly and unexpectedly a little over a year ago. The condo was attractive to us, among many reasons, because it has 1500 square feet on one level with two bathrooms and two bedrooms on a main level and another bedroom/bath suite on a lower level.
I recently convened a meeting with the President of our property management firm to state my desire to “age in place” and to solicit input and support from them as they had previously stated a desire to expand their available (estate) services to the association and residents. I will, myself, take on the process of internal modifications to prepare for the possibility. I, personally, have no desire, if I can avoid, to reside in the typical “nursing home”.
Reply
Jonathan Schroeder - 1984
Very good and timely article. But I cringed a bit to see the term “nursing homes” used. I think too many people have negative ideas about senior living apartments and other facilities for older people, and often lump all options into the “nursing home” category.
Reply