Are your bones up to par?
Half of all women and one in four men over age 50 will break a bone due to osteoporosis.
Osteoporosis is a BIG problem; everyone needs to know about it and how to manage it.
It’s also a costly problem. The disease accounts for 2 million broken bones and $19 billion in related health-care costs annually. By 2025, experts predict osteoporosis will be responsible for approximately 3 million fractures and $25.3 billion in annual costs.
Know your bones
Bone provides shape and support for the body and offers protection for some internal organs. Bone also serves as a storage site for minerals. In addition, our bones provide the medium for developing and storing (red) blood cells.
Like other bodily tissues, bone is a living tissue that comprises the body’s skeleton. There are three types of bony tissues:
- Compact tissue — hard outer tissue of bones
- Cancellous tissue — sponge-like tissue inside of bones
- Subchondral tissue — smooth tissue at the ends of bones, covered with another type of tissue called cartilage.
The periosteum is a tough, thin, hard outer membrane covering all bones. Beneath this shell lie tunnels and canals through which blood and lymph vessels carry nutrients and other materials to and from the bone. In addition, muscles, ligaments, and tendons attach to the periosteum.
The human skeleton consists of 206 bones, not including teeth and small bones located within cartilage. Some 80 axial bones exist in the body. They are in the head, face, auditory system, trunk, ribs, sternum, and hyoid (a horseshoe-shaped bone in the neck between the chin and the thyroid cartilage. It’s the only bone that is not connected to any other nearby bone). There are 126 appendicular bones, which include the arms, shoulders, wrists, hands, legs, hips, ankles, and feet. Bones make up about 12-15 percent of total body weight for most people.
What is osteoporosis?
Osteoporosis means “porous bone” and has become a public health risk due to its severity, chronicity, and progression, which affects mainly postmenopausal women and older adults.
Osteoporosis occurs when the body loses too much bone, makes too little bone, or both. As a result, bones become weak and may break easily from a fall or, in some cases, from sneezing or minor bumps.
Viewed under a microscope, healthy bone (on the left side of the image) looks like a honeycomb. When osteoporosis occurs, the holes and spaces in the honeycomb are much larger than in healthy bone (right side of the image). Osteoporotic bones have less density or mass, with abnormal tissue structure. As bones become less dense, they weaken and are more likely to break.
For most people, a broken bone is often the first sign they have osteoporosis. Another possible sign of the condition is loss of height or a noticeable curvature of the spine.
Who is at risk for osteoporosis?
While people of all races and ethnic groups can develop osteoporosis, certain groups are more likely to develop the disease. Among women, those of white and Asian descent are more likely to develop osteoporosis. Other risk factors include:
- A family history of broken bones or an osteoporosis diagnosis
- History of a broken bone after age 50
- Ovary removal before menstruation stops naturally
- Poor dietary habits, including insufficient amounts of calcium and/or vitamin D
- Physical inactivity or prolonged periods of bed rest
- Cigarette smoking
- Heavy alcohol use
- Altered levels of hormones, such as too much thyroid hormone, too little estrogen in women, or too little testosterone in men
- Long periods of low body weight

One possible sign of osteoporosis is noticeable curvature of the spine. (Image courtesy of Vic Katch.)
Often, other health problems — and a few medical procedures — can increase osteoporosis risk in some people. These include:
- Autoimmune disorders (rheumatoid arthritis, ankylosing spondylitis — see my Health Yourself article “Understanding arthritis” — and multiple sclerosis)
- Digestive and gastrointestinal disorders (celiac disease, inflammatory bowel disease, weight-loss surgery)
- Some cancers (breast, prostate) and blood disorders (leukemia and multiple myeloma, sickle cell disease)
- Neurological disorders, including stroke, Parkinson’s disease, spinal cord injuries
- Blood and bone marrow disorders; various endocrine disorders (diabetes, premature menopause, low testosterone and estrogen in males, hyperthyroidism); and AIDS/HIV
Research suggests that certain medicines taken in large doses for prolonged periods also relate to increased incidences of bone loss. These medicines include:
- Aluminum-containing antacids
- Some antiseizure medicines
- Aromatase inhibitors for breast cancer treatment
- Cancer chemotherapeutic drugs
- Transplant medications
- Some contraception medications
- Proton pump inhibitors
- Some selective serotonin reuptake inhibitors (SSRIs)
- Some steroids
- Some thyroid and hormone medications
- Some steroid medicines
Diagnoses

DEXA scans measure bone density by passing a high- and low-energy X-ray beam through the body. (Image courtesy of A. Weltman, University of Virginia.)
Osteoporosis rarely exhibits overt symptoms. Experts often refer to it as a “silent disease.” Most often, the first indication of osteoporosis is when a minor bump or fall results in a broken bone.
DEXA scans (dual X-ray absorptiometry) measure bone density (thickness and strength of bones) by passing a high- and low-energy X-ray beam (a form of ionizing radiation) through the body, usually at the hip and spine, but also the whole body when prescribed. DEXA scans are safe and pose no health risk. The scan takes about 10 minutes. The person lays still on a platform while a large metal arm passes over the body.
The density profiles from these X-rays are used to calculate bone mineral density. The lower the density, the greater the fracture risk.
Bone densities are scored with a T-score (or a Z-score) as a way to compare a person’s bone density value compared to a reference group value, usually a young adult of the same gender, with peak bone mineral density. If a person’s T-score is 0.0, this means their bone density is the same as the reference group’s bone density. A low bone density T-score would be between -1.0 and -2.5, a condition called osteopenia (low bone density). Osteoporosis identifies as a T-score of -2.5 or higher.
Osteoporosis treatment: The dos and don’ts
Medications for building bone
Bone-building medications are typically reserved for people who have severe osteoporosis and are at high risk for fracture. These medications include Teriparatide (Forteo), Abaloparatide (Tymlos), and Romosozumab (Evenity). These medications require daily or monthly injections and are relatively new, so long-term side effects are unknown. Usually, these drugs are only effective for one or two years, after which their benefits seem to disappear.
Medications may not be enough
At any age, to treat and prevent bone loss, research suggests that, over time, certain lifestyle habits can play a significant role in sustaining bone integrity. Maintaining adequate levels of circulating calcium, Vitamin D, and protein are vital. We can obtain most of these ingredients by eating a well-balanced diet, including fruits, vegetables, and minimal ultra-processed foods.
Calcium-rich food sources
 Men and women between 18 and 50 need 1,000 mg of calcium daily. This increases to 1,200 mg when women turn 50 and men turn 70. The Upper Limit (UL) for calcium is 2,500 mg daily. Too much blood calcium (termed hypercalcemia) can increase the risk of kidney stones, prostate cancer, and constipation.
Men and women between 18 and 50 need 1,000 mg of calcium daily. This increases to 1,200 mg when women turn 50 and men turn 70. The Upper Limit (UL) for calcium is 2,500 mg daily. Too much blood calcium (termed hypercalcemia) can increase the risk of kidney stones, prostate cancer, and constipation.
Whole foods are the best sources of calcium. Dairy products like milk, yogurt, and cheese are high in calcium. Certain green vegetables and other foods contain smaller amounts. Some juices, breakfast foods, soymilk, cereals, snacks, bread, and bottled water feature added calcium. Most versions of plant-based milk are fortified with calcium.
People usually can get enough calcium from food; thus, a supplement may be unnecessary.
There is no added benefit to taking more calcium than needed. But calcium supplements are an option if a person’s diet lacks sufficient variety. If you are going to take a supplement, consider the following:
- Look for labels that state “purified” or have the USP (United States Pharmacopeia) symbol.
- Calcium absorbs best when taken in 500-600 mg doses or less.
- Take (most) calcium supplements with food. Eating food produces stomach acid that helps absorb most calcium supplements. The one exception to the rule is calcium citrate, which can absorb well when taken with or without food.
- Side effects, such as gas or constipation, may occur.
 Vitamin D is a fat-soluble vitamin naturally present in a few foods, added to others, and available as a dietary supplement.
Vitamin D is a fat-soluble vitamin naturally present in a few foods, added to others, and available as a dietary supplement.
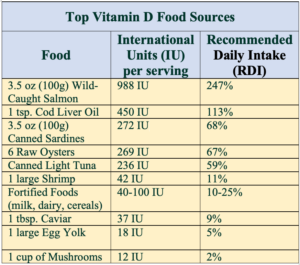
Look for Vitamin D in such fatty fish as wild-caught mackerel, salmon, and tuna. It also is also added to milk, orange juice, soymilk, and fortified cereals, among other things. This list contains foods high in Vitamin D.
Most people need at least 600 international units (IU) of vitamin D daily. The dose increases to 800-1,000 IU daily after age 70. Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol) can supplement a diet deficient in Vitamin D. Both types promote bone health. The supplements can be taken with or without food, and the full amount can be taken at one time.
Vitamin D also produces when ultraviolet (UV) rays from sunlight strike the skin and trigger vitamin D synthesis. But aging skin loses its ability to generate Vitamin D and today’s UV rays are not what they used to be.
Exercise
Exercise helps build strong bones and slows bone loss. Therefore, it is best to combine strength-training exercises with weight-bearing and balance exercises. Strength training helps fortify muscles and bones in the arms and upper spine while weight-bearing exercises — such as walking, jogging, running, stair climbing, skipping rope, skiing, etc. — affect mainly the legs, hips, and lower spine.
Don’t smoke
Recent evidence demonstrates that tobacco smoking causes an imbalance in bone turnover, leading to lower bone mass and making bone vulnerable to osteoporosis. Tobacco smoke indirectly influences bone mass through body weight alteration and increased oxidative stress on bony tissues. Smoking impacts parathyroid hormone-vitamin D axis, adrenal hormones, and sex hormones.
Limit alcohol consumption
Human and animal studies suggest that chronic, heavy drinking, particularly during adolescence and young adulthood, can dramatically compromise bone quality and may increase the risk of osteoporosis with aging. Further, research indicates that the effects of heavy alcohol use on bone cannot be reversed, even if alcohol consumption terminates.
References:
- Aibar-Almazán, A., et al. “Current status of the diagnosis and management of osteoporosis.” The International Journal of Molecular Sciences. 2022;23(16):9465.
- Al-Bashaireh, A.M., et al. “The effect of tobacco smoking on bone mass: An overview of pathophysiologic mechanisms.” Journal of Osteoporosis. 2018;1206235.
- Alcohol and other factors affecting osteoporosis risk in women. National Institute of Health.
- American Bone Health.
- Bhatnagar, A., Kekatpure, A.L. “Postmenopausal osteoporosis: A literature review.” Cureus. 2022;14(9):e29367.
- LeBoff, M.S., et al. “The clinician’s guide to prevention and treatment of osteoporosis.” Osteoporosis International. 2022;33(10):2049-2102.
- “Osteoporosis: National Institute of Arthritis and Musculoskeletal and Skin Diseases.”
- Tonk, C.H., et al. “Therapeutic treatments for osteoporosis — which combination of pills is the best among the bad?” The International Journal of Molecular Sciences. 2022;23(3):1393.
- National Women’s Health Network. “Osteoporosis: Screening and Diagnosis.”







GLENN MARSHALL - 1955E
Excellent article on bone health, thank you Victor.
And sad to say, a doctor wanted me to take medication for my normal bone deterioration
But their answer is always some medication. My friends know that I am healthy, and that I don’t take any prescription meds.
Reply
Russell Lyons - 1983
The article states, “If a person’s T-score is 1.0, this means their bone density is the same as the reference group’s bone density.” This vague statement should be replaced either by “If a person’s T-score is 0.0, this means their bone density is the same as the reference group’s average bone density” or by “If a person’s T-score is 1.0, this means their bone density is larger than the reference group’s average bone density by one standard deviation.” If not replaced, the original statement is confusing.
Reply
Deborah Holdship
Thank you for pointing out this error, which has since been corrected.
Reply
Susan Montgomery - 1984
I was thinking the same thing, Russell.
Reply
Russell Lyons - 1983
Thanks, Deborah, but it would have been even nicer if you had included the word “average”, because the group’s bone density is not well defined: The group has a collection of bone densities, not only one density. That’s the reason I included “average” in both my suggested corrections.
Reply