Moving with intention
Over the years, I’ve discussed the many health benefits of exercise, generally called intentional physical activity. This includes aerobic training, resistance training, or high-intensity interval training. This is different from physical activity (PA), which encompasses exercise as well as typical occupational and/or domestic activity to enhance overall healthspan (the length of time a person is healthy — not just alive). Healthspan encompasses longevity and resilience (the body’s ability to resist, adapt, grow, and recover from different stressors).
Numerous readers have asked why I’ve avoided discussing how, exactly, exercise and PA improve these life-sustaining variables. Because the molecular, cellular, and organistic mechanisms that underlie the beneficial effects of exercise remain scattered, it is challenging to tie together individual research results into one comprehensive and understandable story that speaks to both science and non-science people.
So, in this Health Yourself column, I’ll do my best to briefly tell the emerging story of how exercise and PA may exert their many beneficial health effects. Ready? Put on your high-school biology hat and follow along.
[Note: For simplicity, I use the term “exercise” below to refer to both exercise and PA, recognizing their qualitative differences.]
What are exerkines?
Exerkines are humoral, which is an umbrella term for:
- Substances found in body fluids like blood, cytoplasm, and intra- and extra-cellular fluids, etc.
- Molecular factors, such as peptides (amino acids)
- Metabolites
- Micro-RNAs (miRNAs — small, single-stranded, non-coding RNA, i.e., ribonucleic acid)
- Molecules containing 21-23 nucleotides (basic building blocks of DNA and RNA; found in plants, animals, and some viruses)
- RNA species that are released by cells into the circulation in response to exercise; they are likely to confer multi-systemic exercise effects on different body organs.
For example, it is known that muscles release interleukins (ILs), a group of cytokines (proteins and other signal molecules) that are expressed and secreted by white blood cells (leukocytes) and other cells from different organs (see below). While the significant muscle cytokine released during muscle action is interleukin-6 (IL-6), the number of acute-and-chronic exercise-associated signaling molecules in the human genome includes between 50-100 different cytokines and related proteins secreted by other cells, tissues, and organs in response to exercise.
It is revelatory that in response to acute and chronic exercise, muscle, along with other organs, cells, and tissues, secretes cytokine-signaling molecules!
Specific signaling exerkines have different names related to the specific secreting organ:
- Skeletal muscle = myokines
- Heart = cardiokines
- Liver = hepatokines
- White adipose tissue = adipokines
- Brown adipose tissue = baptokines
- Neurons = neurokines.
Exerkines play potential roles in influencing cell function to improve cardiovascular, metabolic, immune, and neurological health. As such, exerkines demonstrate potent treatment for cardiovascular diseases, type 2 diabetes mellitus, obesity, and certain cancers. They are also believed to facilitate healthy aging.
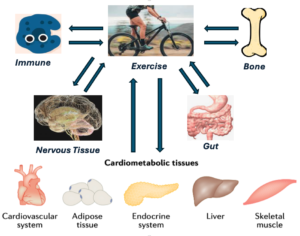
The accompanying figure shows the organs and tissues that serve as exerkine sources are directly influenced by exercise that (it is hypothesized) can result in profound health benefits, including:
- Reducing cardiovascular disease
- Reducing obesity
- Inhibiting cognitive decline
- Inhibiting osteoporosis
- Arresting certain cancers
- Reducing type 2 diabetes, as well as asthma, back pain, arthritis, depression, and dementia.
These exercise-induced effects, cumulatively, positively affect healthspan, longevity, and resilience.
Exerkine influencers … It’s complicated!
Exerkines secrete in response to acute exercise exposure — usually a single aerobic or resistance exercise episode, or chronic, multi-day exercise routines. Chronic exercise also associates with exerkine production during the post-exercise recovery/rest period. Moreover, exerkine responses are influenced by exercise type, duration, underlying fitness level, and the fed-fasting timing status following exercise.Typically, acute exercise associates with exerkine-produced responses focused on metabolic homeostasis, anti-inflammatory mediators, and shifts in fuel use (from carbohydrates to fat).
In contrast, chronic exercise associates with exerkine-produced responses focused on long-term metabolic adaptations and decreased inflammation. When investigating chronic exercise exposure, many variables need to be controlled, including recent dietary composition, fitness level, fed-fasting status, circadian timing, and training modality.
To complicate matters, exerkines are not merely muscle-produced cytokines. They include hormones and neurotransmitters or metabolites associated with exercise, such as catecholamines, lactic acid, or free-fatty acids (fat breakdown molecules). And, of course, there are probably unknown factors that also produce exerkines with endocrine signaling potential.
Yes, it’s complicated!
Let’s get specific
The forefront of most exercise-induced exerkine research details the many exerkine effects produced from different tissue-producing exerkines. Reviewing this research is daunting since the studies are very specific, and it becomes difficult to tie all the data together into an understandable theory. So, I’ll try to summarize what the research tells us about exerkine effects on different body systems.
Cardiovascular system. Exercise mitigates traditional cardiovascular risk factors like obesity and high cholesterol, but these benefits do not account for the benefits of exercise on cardiometabolic health. Studies in human and animal models support a role for exercise-induced exerkines from multiple organs potentially enhancing cardiometabolic health. This occurs via persistent reductions in systemic inflammation, improving dysregulated energy balance and fuel utilization, and increases in blood flow via improvements in vascular endothelial function.
Fat (adipose) tissue. In humans, circulating fat tissue exerkine levels inversely associate with the fat tissue mass amount, fasting insulin, and blood-fat blood levels. Some research also finds that fat tissue-produced exerkines associate with improvements in sugar metabolism, fat breakdown, and a possible reduction in fat-tissue inflammation.
Liver and gut. The liver is recognized as a source of many exercise-circulating proteins. These exerkines affect glucose and/or fat metabolism and alter the gut microbiome, regardless of diet and body weight, while contingent on exercise intensity, modality, and sustainment. The mechanisms by which exerkines might alter the gut microbiome remain controversial, but include altering the gene expression of several gut molecules to produce a more favorable anti-inflammatory profile, improving gut blood flow, or changing bile acid excretion.
Endocrine system. Exercise-induced exerkine excretion from many tissues improves circulating glucose homeostasis, insulin resistance, inflammation reduction, increased fatty acid oxidation, and favorable alterations in glucose homeostasis.
Immune system. Since crosstalk exists between the skeletal muscle and the immune system, most researchers now consider the skeletal muscle to be an immunoregulatory organ that mainly affects lymphocyte and neutrophil trafficking, hence inflammation. Also, exerkine-induced immune effects increase resilience to cancer, co-adjuvant to cancer therapy. Pooled data from 12 studies with self-reported physical activity indicate that increased physical activity levels associate with decreased cancer risk across multiple types. Exercise creates a unique exerkine excretion environment that lasts hours after exercise stops, which most likely represents a window for activation of immune function. For this reason, exercise could potentially serve as a co-adjuvant treatment for cancer therapy.
Nervous system. Current research suggests exercise as a promising non-pharmacological strategy to maintain and improve brain function. The exercise effects on the brain are most apparent in the hippocampus, the part of the brain involved in learning and memory. As such, accumulating evidence suggests exercise can prevent or delay neurodegenerative onset. In my next Health Yourself column, I will report on how exercise and diet can reduce — or even reverse — Alzheimer’s disease.
Bone. It is well known that resistance exercise increases bone mineral density. While multiple mechanisms can explain these results, most notably mechanical loading, other factors are involved, including exercise-associated, bone-derived exerkines.
Conclusions
Contemporary research now recognizes exerkines as critical mediators of the exercise-related changes in health benefits, particularly in the role in inter-organ and systemic communication and coordination. We still need large-scale, structured studies to pursue exerkine-related questions that can predict exercise-produced outcomes, facilitate personalized exercise programs to improve health and reduce disease, and promote resilience across the lifespan.
The bottom line: Move more, sit less, and get your daily dose of exerkines.
References:
Baggish, A.L., et al. “Dynamic regulation of circulating microRNA during acute exhaustive exercise and sustained aerobic exercise training.” The Journal of Physiology, 2011:589,3983.
Chow, L.S., et al. “Exerkines in health, resilience, and disease.” Nature Review: Endocrinology, 2022;18:273.
Cullen, T., et al. “Interleukin-6 and associated cytokine responses to high-intensity interval exercise: The effect of exercise intensity and volume. Applied Physiology, Nutrition, and Metabolism, 2016;41,803.
Erickson, K.I., et al. “Exercise training increases size of hippocampus and improves memory.” Proceedings of the National Academy of Sciences of the United States of America, 2011;108,3017.
Horowitz, A.M., et al. “Blood factors transfer beneficial effects of exercise on neurogenesis and cognition to the aged brain.”
Science, 2020;369,167.
Jia, S., et al. “Exerkines and osteoarthritis.” Frontiers in Physiology, 2023;14:1302769
Jin, L, et al. “Exerkines and cardiometabolic benefits of exercise: From bench to clinic.” EMBO Molecular Medicine, 2024;16(3):432-444.
Moore, S.C., et al. “Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults.” JAMA Internal Medicine, 2016;176,816.
National Heart, Lung, and Blood Institute. NHLBI and NIDDK Workshop: Exerkines in health, resilience, and diseases executive summary,(2020).
Nicolini, C., et al. “A single bout of high-intensity interval exercise increases corticospinal excitability, brain-derived neurotrophic factor, and uncarboxylated osteolcalcin in sedentary, healthy males.” Neuroscience, 2020;437,242.
Ostrowski, K., et al. “Pro- and anti-inflammatory cytokine balance in strenuous exercise in humans.” The Journal of Physiology, 1999;515,287.
Robbins, J.M., Gerszten, R.E. “Exercise, exerkines, and cardiometabolic health: From individual players to a team sport.” The Journal of Clinical Investigation, 2023;133(11):e168121. Erratum in: J Clin Invest 2023;133(13):e172916.
Safdar, A., et al. “The potential of endurance exercise-derived exosomes to treat metabolic diseases.” Nature Reviews Endocrinology, 2016;12, 504.
Sanford, J.A., et al. “Molecular transducers of physical activity consortium (MoTrPAC): Mapping the dynamic responses to exercise.” Cell, 2020;181,1464.
Segar, M.L., Katch, V.L., et al. “The effect of aerobic exercise on self-esteem and depressive and anxiety symptoms among breast cancer survivors.” Oncology Nursing Forum, 1998;25(1):107.
Stanford, K.I., et al. 12,13-diHOME: “An exercise-induced lipokine that increases skeletal muscle fatty acid uptake.” Cell Metabolism, 2018;27,1357.
Steensberg, A., et al. “Production of interleukin-6 in contracting human skeletal muscles can account for the exercise-induced increase in plasma interleukin-6.” Journal of Physiology, 2000;529,237.
Takahashi, H., et al. “TGF-β2 is an exercise-induced adipokine that regulates glucose and fatty acid metabolism.” Nature Metabolism, 20191,291.
Zhou, N., et al. “Exploring exercise-driven exerkines: Unraveling the regulation of metabolism and inflammation.” PeerJ, 2024;12:e17267.




Russell Lyons - 1983
While I think that exercise is great, the statement “It is well known that resistance exercise increases bone mineral density” deserves some qualification. Apparently, there is little good evidence of this. The Cochrane review (https://www.cochrane.org/CD000333/MUSKEL_exercise-for-preventing-and-treating-osteoporosis-in-postmenopausal-women) says this:
“The review shows that for postmenopausal women
– Exercise will improve bone mineral density slightly.
– Exercise will reduce the chances of having a fracture slightly.
These results might have happened by chance.”
Reply
Victor Katch
Russell, thank you for your comments. As you point out, resistance-exercise effects on bone mineral density and bone status (osteopenia/osteoporosis versus normal bone) may be small-to-moderate, on average. Nevertheless, based on robust statistical methods using systematic reviews and meta-analyses involving hundreds of studies using thousands of men and women, the exercise effects are greater then a chance occurrence. Therefore, resistance exercise is recommended for increasing and/or preventing loss of bone density for most individuals.
Reply