Achin’ for you
Arthritis means inflammation or swelling in one or more joints and is most common in the feet, hands, hips, knees, and lower back (spine).
More than 100 arthritic subtypes affect people regardless of age, race, and gender. Arthritis is the leading cause for disability in the U.S. The disease is more common among women than men, and while it is not an aging disease, some types occur more often in older people.
Arthritis Prevalence
- In 2020, an estimated 22.3 percent of all U.S. adults 18 or older had some arthritis.
- Women have a higher age-adjusted arthritis prevalence than men. At least 1 in 4 women report having arthritis.
- The percentage of adults with arthritis in 2020 varied by state, ranging from 18.1 percent in Hawaii to 32.8 percent in West Virginia. Michigan reported 26.5 percent of adults had doctor-diagnosed arthritis in 2020.
- Arthritis prevalence increases dramatically in persons with comorbidities (the simultaneous presence of two or more diseases or medical conditions). Individuals who are overweight or obese, or who have conditions that limit physical activity, are especially at risk.
Long-term burden
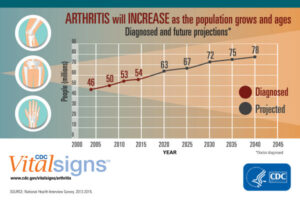
This graph from the National Health Interview Survey 2013-15 shows arthritis will increase as the population grows and ages. (Credit: CDC.)
Most alarming, researchers predict arthritis prevalence will increase in the coming decades (see graph). By the year 2040, an estimated 78.4 million adults over the age of 18 will have doctor-diagnosed arthritis, and two-thirds are expected to be women. Moreover, by 2040, an estimated 34.6 million adults will report limitations in activity attributed to arthritis.
What’s your type?
The most common types of arthritis include:
- Osteoarthritis (OA) – The “wear and tear” arthritis, which develops when joint cartilage breaks down from repeated stresses.
- Rheumatoid arthritis (RA) – An immune system disease that attacks joint synovial membranes (impacting connective tissues and joint lubrication).
- Psoriatic arthritis – A joint inflammation disease that develops in people with psoriasis (the autoimmune disorder that causes skin irritation).
- Gout –The disease that causes hard uric acid crystals to form in joints, most often the feet.
- Ankylosing spondylitis (AS) – An inflammatory arthritic condition that affects joints and ligaments in the lower back resulting in the fusion of vertebrae in the spine.
- Juvenile idiopathic arthritis (JIA) – An immune system disorder that typically affects children 16 or younger.
Let’s break it down
Osteoarthritis (OA)
OA represents that most prevalent arthritis type occurring most often in overused joints that bear weight. (Stock image.)
OA represents the most prevalent arthritis type. It occurs most often in overused joints that bear weight: knees, hips, feet, and spine. It also can arise from injury or when there is extra stress on the joints, as occurs in long-term obesity.
Symptoms
- Pain in affected joints, especially with movement.
- Stiffness, most noticeable following inactivity.
- Tenderness when pressure is applied on or near the joint.
- Joint swelling.
- Grating, popping, or cracking sensations during movement.
- Bone spurs, which feel like lumps below the skin around an OA-affected joint.
Rheumatoid Arthritis (RA)
RA represents an autoimmune disease in which the immune system malfunctions and attacks healthy tissue. RA is one of about 80 different types of autoimmune diseases.
Symptoms: RA symptoms can come on gradually or start suddenly.
- About 1 in every 5 people who have RA experience lumps on their skin called rheumatoid nodules. These nodules often form over joint areas that receive pressure, such as knuckles, elbows, or heels.
- Pain, stiffness, and swelling in multiple joints: hands, wrists, elbows, shoulders, knees, ankles, feet, jaw, and neck. There appears to be no common symptom pattern from joint to joint.
- Morning stiffness that can last for a few hours, or all day.
- Extreme fatigue with decreased appetite and weight loss.
Psoriatic Arthritis
This arthritis type involves your skin (psoriasis) and joints (arthritis). It usually initiates between ages 30-50, but it can start as early as childhood. It’s equally common among men and women. Psoriasis usually appears first.
Symptoms: Psoriasis causes patchy, raised, red, and white inflamed skin areas with scales. It usually affects the tips of the elbows and knees, the scalp, the navel, and skin around the genital areas or anus. It can also affect the fingers and toes. People who have psoriasis often have pitted or discolored fingernails. In some people, only one joint becomes affected.
Gout

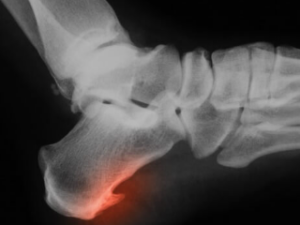
Gouts’ major symptom can appear suddenly– a person wakes up with a sudden, intense pain in the big toe. (Stock image.)
Gout involves uric acid crystal build-up inside a joint, usually the big toe. In gout, the body produces more uric acid than needed (termed hyperuricemia). Uric acid produces when purine (found in many foods) in the body breaks down into uric acid. There are two kinds of purine: endogenous and exogenous. Endogenous purines are made directly by the body while exogenous purines are absorbed by the body from food. Eating too many purines can cause uric acid buildup. If uric acid remains in the body, it can crystallize and cause arthritis (or diabetes or kidney failure).
Foods with high purine content include organ meats such as goose, veal, turkey, and venison — that’s why gout was known in the Middle Ages as the “rich man’s disease.” Other problematic foods include seafood — particularly sardines and anchovies, herring, scallops, mussels, codfish, tuna, and haddock. Alcohol and high-fructose-sweetened beverages are also culprits.
Symptoms: Gout’s major symptom can appear suddenly – a person wakes up with intense pain in the big toe. The attack can last between three and 10 days, and may return at any time. Over time, the attacks grow more frequent and last longer.
Ankylosing Spondylitis (AS)
AS represents an inflammatory disease that can cause chronic spinal bone fusion. This fusion makes the spine less flexible resulting in a hunched posture. If ribs are affected, it can also make deep-breathing difficult. The cause for AS is still unclear, but it does seem to run in families, possibly linked to the HLA-B27 gene, present in fewer than 8 percent of the general population.
Symptoms: AS signs and symptoms typically begin between the ages of 17 and 45, and include pain and stiffness in the lower back and hips, especially in the morning and after inactivity. Neck joint pain and fatigue also are common, as is appetite loss, unexplained weight loss, skin rashes, and vision problems. Areas most commonly affected include the joint between the base of the spine and the pelvis, the vertebrae in the lower back, the hip and shoulder joints, and the cartilage between the breastbone and the ribs.
Juvenile idiopathic arthritis

JIA represents several different chronic disorders involving joint inflammation which causes joint pain, swelling, warmth, stiffness, and motion loss. (Stock image.)
JIA is so named because its origins are not understood. It represents several different chronic disorders involving joint inflammation, which causes joint pain, swelling, warmth, stiffness, and motion loss. The various JIA forms have different features.
Symptoms: JIA symptoms vary depending on the type, but all forms share persistent joint pain, swelling, warmth, and stiffness that are typically worse in the morning and after a nap or prolonged sitting. One early JIA sign may be limping in the morning due to disease in one or both legs. JIA symptoms go through cycles, flaring for a few weeks or months followed by remissions.
Other common JIA systems include eye inflammation (oligoarticular JIA), skin changes, daily fever bouts, and growth problems including limb differential growth patterns causing one leg or arm to be longer than the other.
Treatment options
Arthritis conditions are generally not curable but are manageable. Treatment focuses on symptom management, preventing further damage, and improving quality of life.
Short-term home remedy treatments include:
- Medications – nonsteroidal anti-inflammatory drugs (NSAIDs) and pain relievers (acetaminophen, aspirin, ibuprofen, or other anti-inflammatory-type medications) can be helpful.
- Counterirritants – some creams and ointments contain menthol or capsaicin (the ingredient found in hot peppers), which can interfere with pain signal transmission from the joint.
- Heat and cold – using moist heat (warm bath or shower), dry heat (heating pad), or cold compresses can help with pain management.
- Joint immobilization – a splint or brace can help a joint rest and protect it from further injury.
- Massage – light massage of painful muscles may increase blood flow and reduce pain.
- Epsom salt baths can sometimes offer all-over pain relief.
- Transcutaneous electrical nerve stimulation (TENS) – a TENS device, which sends mild, electrical pulses to nerve endings in the painful area, can be helpful in reducing pain perception.
- Acupuncture may stimulate pain-relieving chemicals.
- Hot and cold compresses can soothe stiff joints, relax muscles, and ease inflammation.
- Various support and assistive devices can take pressure off affected joints. People often use braces, canes, gripping tools, and taping.
Long-term treatments include:
- Disease-modifying antirheumatic drugs (DMARDs) – These prescription medications (methotrexate, hydroxychloroquine, sulfasalazine, and chlorambucil) can slow down disease progression and treat any immune system-linked issues.
- Steroids – Corticosteroids taken orally or as an injection can help reduce inflammation and swelling.
- Hyaluronic acid – Injecting hyaluronic acid into an affected joint often relieves symptoms.
- Surgery – Options include arthroscopy, fusion, or joint replacement.
Physical Therapy
Exercise can improve range-of-motion and strengthen the muscles surrounding joints. In some cases, splints or braces may be warranted.
Lifestyle Changes
Exercise also can ease pain and help improve and maintain posture. Good posture can help avoid spine problems and reduce pain and stiffness. Smoking cessation has been found to reduce arthritic symptoms.
Are prevention and reversal possible?
A major breakthrough in arthritis prevention research recently was published. This study identified Talarozole, a drug known to increase retinoic acid (made in the body from vitamin A to help cells grow and develop) was successfully used to prevent osteoarthritis in disease models (in animals and humans) by blocking or suppressing the genes in joint cartilage after 26 days of administration.
While still at an early stage, this research reveals encouraging findings for a new class of disease-modifying drugs to treat osteoarthritis.
References
- Arthritis Foundation.
- Arthritis Statistics.
- Centers for Disease Control and Prevention.
- Hootman, J.M., et al. “Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults,”
2015-2040. Arthritis Rheumatology, 2016;68(7):1582. doi:10.1002/art.39692. PubMed PMID: 27015600. - Kim, K.H., et al. “Familial risk of gout and interaction with obesity and alcohol consumption: A population-based cohort study in Korea. Arthritis Care & Research (Hoboken). 2023 Jan 30. doi: 10.1002/acr.25095. Epub ahead of print. PMID: 36714912.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. Arthritis.
- Palomino-Tapia, V., et al. “Review of Viral Arthritis in Canada.” Avian Diseases. 2022 Dec;66(4):452-458.
- Suzgun, M.A., et al. “A review of rheumatoid meningitis with case studies.” Modern Rheumatology Case Reports. 2023 Jan 31:rxad010. doi: 10.1093/mrcr/rxad010. Epub ahead of print. PMID: 36718604.
- Versus Arthritis. All about arthritis.
- Zhu, L., et al. “Variants in ALDH1A2 reveal an anti-inflammatory role for retinoic acid and a new class of disease-modifying drugs in osteoarthritis.” Science Translational Medicine. 2022;21;14(676):eabm4054.







richard DSouza - 1974
I am currently 73 years old and have arthritis mainly in my thumb joints, which is more of an annoyance than anything else. Your article was very informative . thanks,
Richard
Reply
Bryan O'Rear - 2001
This article was a very useful reminder for our trainers to maintain JIA on their radar when working with groups of youth athletes. This demographic is greatly impacted. Providing context of where JIA lives among the broader Arthritis landscape is also always helpful where early diagnosis is so essential. Thank you !
Reply