Overcoming public health challenges
For centuries the major focus of medical research has been to reduce communicable diseases like hepatitis, HIV/AIDS, malaria, polio, and tuberculosis, to name a few. An investment of considerable public monies has led to great scientific discoveries, and many horrible diseases have faded into history. Many people under the age of 40 have never come across individuals with TB or polio, or even know what an “iron lung” is.
Eradicating communicable diseases represents one of western medicine’s greatest success stories. As a society, we have reduced the spread of communicable diseases through several public health initiatives:
- Protecting and cleaning public water supplies
- Improving public sanitation
- Providing safe food-packaging procedures
- Monitoring and regulating food production
- Improving transportation and storage
- Curtailing pesticide and hormone use around foods
- Providing for public protection of air quality
All of these efforts have significant impacts on the promotion of long-term health.
Meanwhile, most private-sector efforts to address infectious diseases have centered on discovery of new drug treatment options. While this costs enormous amounts of money, it also results in vast profits for those few companies with resources and willingness to participate.
The industrial epidemic of non-communicable diseases
The daunting public health challenge today is to reduce incidences of noncommunicable diseases (NCDs), such as heart disease, diabetes, stroke, some cancers, and obesity. NCDs now represent the leading causes of death for most populations around the world.However, unlike communicable diseases where considerable public consensus exists to intervene to reduce microbial causes of pestilence and famine, garnering support to reduce underlying causes of NCDs has proven more elusive. Efforts often are undermined by the very industries that cause major NCDs. Additionally, at least in the U.S., public appetite for government regulations of any kind is at an all-time low.
Salt, sugar, fat

“If you had any doubt as to the food industry’s complicity in our obesity epidemic, it will evaporate when you read this book.” — The Washington Post
There seems little doubt that sale and use of “unhealthy commodities,” primarily tobacco, alcohol, and ultra-processed foods and sugary drinks, are major causes of the global epidemic of NCDs. While restrictions and regulations regarding advertising, sales, and distribution of tobacco (and to some extent alcohol) have been underway for a few decades with some success, such is not the case with ultra-processed food and drink.
Ultra-processed products are created from substances extracted or refined from whole foods. Such products include oils, hydrogenated oils and fats, flours and starches, variants of sugar, and cheap parts or remnants of animal foods — with little or no whole foods.
Examples of ultra-processed foods include pre-made, processed burgers, frozen pizza and pasta dishes, chicken nuggets, cereal bars, carbonated and other sugared drinks, and various confectionary and snack products.
Most are made, advertised, and sold by large transnational corporations and are very durable. They tend to taste good, and are ready to consume, which is an enormous commercial advantage over whole or minimally processed foods. Consequently, ultra-processed food production and consumption is rising quickly worldwide. In North America and Europe, principally, ultra-processed products have largely replaced dietary patterns based on fresh, whole, and minimally processed foods that have less fat, sugar, and salt. In the global south — Asia, Africa, and Latin America — ultra-processed products are beginning to displace established dietary patterns that were in place for centuries, and it appears there is no way to stop this juggernaut.
Ultra-processed products are typically energy-dense with a high glycemic load that causes a rapid raise in blood sugar. They are low in dietary fiber, micronutrients, and phytochemicals. And they are high in unhealthy types of dietary fat, free sugars, and sodium. (See: Health Yourself – The manufactured sodium controversy.)
When consumed in small amounts and with other healthy sources of calories, these products are probably harmless. However, intense palatability achieved by high fat, sugar, and salt content (and other additives), along with aggressive marketing strategies like reduced cost for super-sized servings, all make modest consumption of ultra-processed products unlikely. Ultra-processed products are now displacing fresh or minimally processed foods from the family table, leading to energy overconsumption and reductions in fiber, phytochemicals, vitamins, minerals, and, in many cases, protein.
Corporate disease peddlers
Studying the effect of corporate behavior on health is an emerging area of public health research – it studies health risks caused by transnational corporations and the distribution of the unhealthy commodities they market. These corporations profit from sales of unhealthy commodities and many will deny at every opportunity any relationship between the products they pedal and their health-outcome effects.There is evidence that many of these corporations hire professionals to posit opinions, position papers, and reviews intended to mislead, misdirect, and confuse the public about the potential health risks of their products. And finally, they hire lobbyists to influence and give financial support to politicians of any political persuasion to avoid public scrutiny, debate, and regulation. This is the same game plan with the same tactics used by tobacco in the 1980s and 1990s.
Transnational penetration
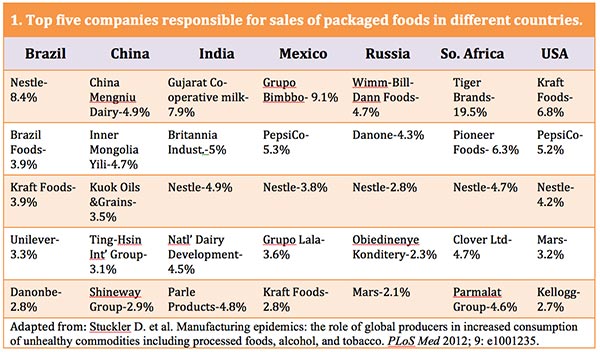
Table 1 below shows the top-five companies responsible for sales of packaged foods in Brazil, China, India, Mexico, South Africa, Russia, and the U.S. With the exception of China, there is a high degree of transnational penetration into the food systems of low-income and middle-income countries, similar to that in the U.S.
In fact, there is little competition in the marketplace. In the U.S. for example, the 10 largest food companies control more than half of all food sales. Worldwide these same companies control about 15 percent of the total market, and it is rapidly rising. For example, Kraft Foods, the main seller of packaged food in the U.S., is responsible for about 6.8 percent of all sales here, and Nestle already has 8.4 percent of all packaged-food sales in Brazil. An even higher degree of concentration is evident for sales of specific categories of ultra-processed products by only a few transnational companies.
Similarities between strategies used by the tobacco, alcohol, and food and drink corporations are striking. There are histories of joint ownership — for example, Philip Morris at one time owned both Kraft and Miller Brewing; Altria was a lead shareholder in tobacco and food companies that have shared directorships. The board at SAB Miller includes at least five past or present tobacco company executives and board members. Additionally, tobacco and food and drink corporations use many of the same public relations firms to lobby worldwide and to design their marketing campaigns.
Targeting low- and middle-income countries
The effects of unhealthy commodities on health outcomes are well documented. In 2010 alone, tobacco was responsible for more than 6.3 million deaths worldwide; alcohol accounted for 4.9 million deaths. Combined, this represents about 12 percent of global disability-adjusted life-years. In addition, high blood pressure, obesity, diabetes, and high blood lipids — all of which directly relate to consumption of ultra-processed foods and sugary drinks — cause more than 18 million deaths every year. And most disturbing, almost all sales growth of these commodities is occurring in low- and middle-income countries, since high-income countries are quickly reaching moderate-to-high sales saturation.
Table 2, below, displays the annual growth rate of volume consumption of ultra-processed foods per person in low-, middle- and high-income countries between 1997-2009. (These are the most recent published data).
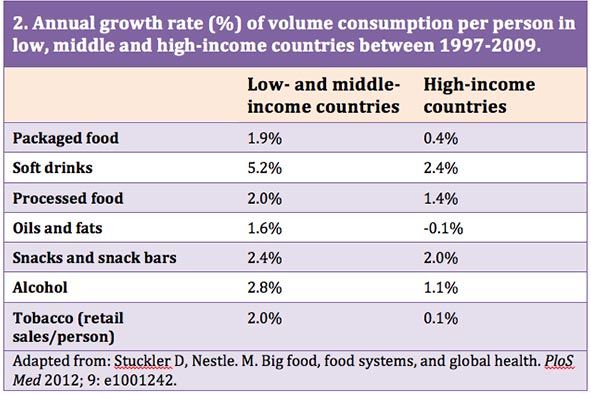
The transition from traditional diets of whole or minimally processed foods to highly processed foods and drinks is quickly accelerating, driven of course, by the transnational “disease peddlers.” The growth of ultra-processed foods and drinks parallels the rates of increase in cardiovascular disease, obesity, diabetes, and other diet-related chronic diseases. As can be seen in the table, sales of ultra-processed food and drink products are rising most rapidly in low- and middle-income countries. This is a serious problem and suggests rising rates of chronic disease in the very countries that are least able to handle the growing number of sick people who will require long-term medical care.
Disease peddlers’ game plan
There are four main strategies used by transnational food and beverage industries to continue to peddle their products.
First, they hire academics and medical doctors to publish ghostwritten studies purporting to negate links between commodities sold and any health risks. Like tobacco, they create quasi-independent organizations to publish biased and partial scientific reports that deny harm, and suppress health information. In last month’s Health Yourself — Industry funding: Pros and cons, I presented research showing systematic bias from industry funding. (Studies sponsored exclusively by food and drink companies are four to eight times more likely to have conclusions favorable to the financial interests of the sponsoring company than those with no funding.)
The second strategy is to co-opt policymakers and health professionals. Like tobacco, the food and drink industries try to “hook” customers as young as possible, using tactics such as early-childhood health promotion schemes. Also, these companies try to forge alliances with legislators and government officials to help participate in formulating national control policies that expressly serve their interests. For example, SAB Miller – the world’s second-largest brewer measured by revenue – and the International Center for Alcohol Policies have assisted the Malawi, Uganda, and Botswana governments to write their national alcohol-control policies.The third strategy is to lobby politicians and public officials to oppose any regulations. The alcohol and ultra-processed food and drink corporations wield enormous power. According to U.S. Senate records, the largest alcohol companies spent $150 million lobbying between 1999-2011. The U.S. Senate Office of Public Records shows that PepsiCo, alone, reported spending more than $9 million in 2009 to lobby the U.S. Congress. In the 2008 election cycle, the company’s Political Action Committee, ironically named “The Concerned Citizen Fund,” contributed $547,700 to candidates who were “pro-business,” and who were committed to improving PepsiCo’s business climate. In another example, the Sugar Association threatened the World Health Organization (WHO) that it would lobby the U.S. government to withdraw its funding because WHO’s strategy on diet, physical activity, and health highlighted a strong link between sugar and NCD risk.
The fourth strategy is to encourage voters to oppose all regulations dealing with food and beverages. The mantra is to emphasize that food and beverage use are an individual responsibility. Moreover, “blame-the-victim” campaigns reduce public support for government interventions. As an alternative, the transnational food industries promote ineffective individually targeted information and educational approaches. Marketing emphasizes personal choice and responsibility and portrays “nanny government” intervention as coercive and oppressive. These industries also avoid disclosure of relevant health information to consumers and block access to objective health information.
Finally, to deflect criticism, transnational corporations promote actions outside their areas of expertise. For example, the ultra-processed food and drink corporations emphasize physical inactivity. They hope that by promoting feel-good projects favorable to consumers they can manipulate public opinion.
Lightening the global burden
There are three approaches to address the disease burden caused by unhealthy commodities:
- Voluntary self-regulation
- Public–private partnerships
- Regulation and market intervention
Industry-supported, voluntary self-regulation represents the default approach of many governments and, of course, is the preferred approach of the food-and-beverage industry. Transnational corporations argue that market forces driven by informed individual choice can nullify any negative results caused by high consumption of unhealthy commodities.
Public–private partnership is based on the belief that government association with industry will lead to greater success than does expecting industry to act independently of regulatory agencies. It can be argued that since not all processed foods are unhealthy, partnership with industry might lead to reformulation of some products to less unhealthy compositions. Many public–private partnerships exist — e.g., the recently announced three-year partnership between the International Diabetes Federation and Nestle (2012). There is no objective evidence, however, that this approach delivers benefits to the consumer.
The third approach is to enforce public, statutory regulations similar to those used to control firearms (in some countries), road traffic, drugs, and tobacco, and to protect parks, forests, and open spaces. The threat and action of government regulation is the only way to change transnational corporation behavior. Thus, the audience for public health is government, not industry.
It is my opinion that unhealthy commodity industries should have no role in formation of national or international policy for NCDs. Public approaches such as legislation, regulation, taxation, pricing, ban, and restriction of advertising and sponsorship need to be employed to promote public health.
Finally, as much as possible, vote with your pocketbook and don’t purchase these items, if possible – this approach always works in the long run.
References
- Alexander, E., et al. 2011. “Major multinational food and beverage companies and informal sector contributions to global food consumption: Implications for nutrition policy.” Global Health; 7:26.
- Basu, S., et al. 2012. “Nutritional determinants of worldwide diabetes: an econometric study of food markets and diabetes prevalence in 173 countries.” Public Health Nutrition; 13:1.
- Bond, L., et al. 2010. “Selling addictions: similarities in approaches between Big Tobacco and Big Booze.” Australasian Medical Journal; 3:325.
- Brownell, K.D., Warner, K.E., 2009. “The perils of ignoring history: Big Tobacco played dirty and millions died. How similar is Big Food?” Milbank Quarterly; 87:259.
- Brownell, K.D., 2012. “Thinking forward: The quicksand of appeasing the food industry.” PLoS Medicine; 9(7):e1001254.
- Center for Responsive Politics. 2010. “PepsiCo Inc. fundraising/spending by cycle.”
- Freedhoff, Y., et al. 2011. “Partnerships between health organizations and the food industry risk derailing public health nutrition.” Canadian Medical Association Journal; 183, no. 3.
- Hawkes, C., 2003. “Marketing activities of global soft drink and fast food companies in emerging markets: A review.” Globalization, diets and noncommunicable diseases. Geneva: World Health Organization.
- Jahiel, R.I., 2007. “Industrial epidemics, public health advocacy, and the alcohol industry: Lessons from other fields.” Addiction; 102:1335.
- Joint WHO/FAO Expert Consultation. 2003. “Diet, nutrition, and the prevention of chronic diseases.” WHO Technical Report Series 916. Geneva: World Health Organization.
- Lawrence, F., 2010. “Who is the government’s health deal with big business really good for? The Guardian.
- Lim, S.S., et al. 2010. “A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study.” Lancet; 380:2224.
- Lincoln, P., et al. 2011. “Conflicts of interest and the UN high-level meeting on non-communicable diseases.” Lancet; 378: e6.
- Lipton, E., 2015. “Food industry enlisted academics in G.M.O. lobbying war, emails show.” New York Times, 9/6/2015.
- Ludwig, D.S., 2011. “Technology, dirt, and the burden of chronic disease.” Journal of the American Medical Association; 305:1352.
- Lyson, T. 2000. “Stalking the wily multinational: Power and control in the U.S. food system.” Agriculture and Human Values; 17:199.
- Malik, V., et al. 2010. “Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk.” Circulation; 121:1356.
- Monteiro, C.A., Cannon, G. 2012. “The impact of transnational ‘big food’ companies on the South: A view from Brazil.” PLoS Medicine; 9:e1001252.
- Monteiro, C.A., et al. 2011. “Increasing consumption of ultra-processed foods and likely impact on human health: Evidence from Brazil.” Public Health Nutrition; 14:5.
- Monteiro, C.A., 2011. “The big issue is ultra-processing. There is no such thing as a healthy ultra-processed product.” World Nutrition; 2:333.
- Moodie, R., et al. [On behalf of The Lancet NCD Action Group]. 2013. “Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries.” Lancet; 381:670.
- Neal, B., 2013. “Fat chance for physical activity.” Population Health Metrics; 11:9.
- Nestle, M., 2013. Food Politics: How the Food Industry Influences Nutrition and Health. 3rd ed. Berkeley: University of California Press.
- O’Connor, A., 2015. “Coca-Cola funds scientists who shift blame for obesity away from bad diets.” New York Times, 8/9/15.
- Phillip Morris, 1999. “Proposal for the organisation of the Whitecoat Project.”
- Popkin, B., 2011. “Agricultural Policies, Food, and Public Health.” EMBO Reports; 12(1):11.
- Shah, A., “PepsiCo taps Edelman to lead multimillion-dollar campaign.” 2009.
- Simon, M., 2015. “Nutrition scientists on the take from Big Food: Has the American Society for Nutrition lost all credibility?”
- Slade, J., 1989. “The tobacco epidemic: Lessons from history.” Journal of Psychoactive Drugs; 21:281.
- Stuckler, D., et al. 2011. “Global health philanthropy and institutional relationships: How should conflicts of interest be addressed?” PLoS Medicine; 8:e1001020.
- Stuckler, D., et al. 2012. “Manufacturing epidemics: The role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco.” PLoS Medicine; 9: e1001235.
- Stuckler, D., Nestle, M. 2012. “Big food, food systems, and global health. PLoS Medicine; 9:e1001242.
- U.N. General Assembly. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. 2011.
- U.S. Senate Lobbying Act Disclosure Database. 2012.
- WHO, 2011. “Global status report on noncommunicable diseases 2010.” Description of the global burden of NCDs, their risk factors, and determinants. Report. Geneva: World Health Organization.
- Wiist, W.H., 2012. “The corporate playbook, health, and democracy: The snack food and beverage industry’s tactics in context.” In: Stuckler D., Siegel, K., eds. “Sick societies: responding to the global challenge of chronic disease.” Oxford: Oxford University Press; 204–16.


