Making connections
In last month’s “Health Yourself” column I discussed possibilities that individuals with similar personality traits were more likely to develop certain illnesses. I suggested perhaps there exists a generic disease-prone personality “type” that increases susceptibility to various diseases.
The connection between personality and disease is not simple. But as more and more research accumulates, a clearer picture emerges of relationships between personality and disease. Most of the research suggests people with specific personality types cope with stress differently, resulting in different patterns of stress-induced disease, influenced by genetics, of course.
The four humors
Extensive literature exists on the topic of classifying various types of human temperaments and labeling them as personality traits or types. These classification systems attempt to describe predominant features of specific personalities that differentiate among individuals. One of the early attempts at classifying personality types was the four humors theorythat had its origins in ancient Egypt.
Greek physician Hippocrates (460-370 BC) developed the humors idea into a medical theory. He believed certain human moods, emotions, and behaviors were caused by an excess or lack of body fluids (called “humors”): blood, yellow bile, black bile, and phlegm. Having the correct balance of humors determined susceptibility to certain diseases.
Prominent Greek physician Galen of Pergamon (AD 129-c. 200) proposed the first typology of temperament based on the four humors model. In his writings De temperamentisGalen classified the human temperament into hot/cold and dry/wet categories. In this system a “balance” could exist between the qualities, yielding a total of nine temperaments.
Four of these categories were named sanguine, choleric, melancholic, and phlegmatic, respectively. According to Galen, each of these categories associated with specific behavior patterns and diseases. This medical “model” was used well into the 17th century as a way of explaining disease.
- The sanguine temperamentassociates with air. People with this temperament, according to Galen, tend to be lively, sociable, carefree, talkative, and pleasure-seeking. They are warm-hearted and optimistic and make new friends easily. They are imaginative and artistic. Sanguine personalities struggle with following tasks all the way through and are chronically late or forgetful.
- Galen’s choleric temperamenttraditionally associates with fire. People with this temperament tend to be egocentric and extroverted. They are excitable, impulsive, and restless, with reserves of aggression, energy, and/or passion. Choleric individuals are usually task-oriented and focused on getting a job done efficiently. They can be ambitious, strong-willed, and like to be in charge. They demonstrate leadership, are good at planning, and tend to be practical and solution-oriented. They appreciate receiving respect and esteem for their work.
- The melancholic temperamenttraditionally associates with the earth element. People with this temperament appear serious, introverted, cautious, or even suspicious. They can become preoccupied with the tragedy and cruelty in the world and are susceptible to depression and moodiness. They may be focused and conscientious. They often prefer to do things themselves, both to meet their own standards and because they are not inherently sociable.
- The phlegmatic temperamenttraditionally associates with water. People with this temperament are inward and private, thoughtful, reasonable, calm, patient, caring, and tolerant. They tend to have a rich inner life, and seek a quiet, peaceful atmosphere. They are content with themselves. They tend to be steadfast and consistent in their habits, and make steady and faithful friends. People of this temperament appear somewhat ponderous or clumsy, and their speech tends to be slow or appear hesitant.
Fast forward
 The four humors theory has changed and morphed since Galen’s time, but the idea persists that personality types and traits link to disease. And now research exists explaining how the different temperaments may precipitate disease.
The four humors theory has changed and morphed since Galen’s time, but the idea persists that personality types and traits link to disease. And now research exists explaining how the different temperaments may precipitate disease.
About five decades ago cardiologists R. Rosenman and M. Friedman observed those who contracted heart disease exhibited “an action-emotion complex that can be observed in any person who is aggressively involved in a chronic, ceaseless, never-ending struggle to achieve more and more in less and less time, and if required to do so, against the opposing efforts of other things or other people.” This struggle against time and people, it was argued, is precisely what precipitates heart attacks. They called it the “hurry sickness” and began a series of studies to identify how this temperament could link to heart disease.
The landmark Western Collaborative Group Study involved more than 3,000 men in their 40s and 50s who did not show any signs of existing coronary heart disease at the onset of the study. After an eight-year follow-up, those men identified with the “hurry-sickness” personality were more than twice as likely to get heart disease as those who had not exhibited the same traits, according to the study.
Originally, these men were said to have a coronary disease-prone personality, but the termed was changed to Type A personality. In 1981 the National Heart, Lung, and Blood Institute concluded that Type A behavior represented an independent risk factor of cardiovascular disease. Of course, not all research supports these findings and many studies showed that some components of Type A behavior were relatively harmless, while others, called the toxic core of Type A personality traits, predicted coronary disease with a high degree of accuracy.
Toxic core traits of the coronary disease-prone personality
The following five temperament traits create major health risks for people of all personality types, but are most potent for the coronary disease-prone personality. Each of these traits relate directly to biological and psychological increases in the “stress response.”
- Hostility, a primary trait of Type A behavior, represents a permanent, deep-seated anger that hovers quietly until some trivial incident causes it to rupture to the surface in a burst of hostility. That hostility is characterized by expressions of anger, the tendency to argue in a loud voice, and the potential for physical aggression when provoked. Hostility not only presents in speech and physicality, but also in one’s mind. Always thinking negatively, holding grudges, and blaming wrongdoings on others are examples of hostility.
- Anger defines as an emotional state incorporating feelings ranging from irritation and aggravation to rage and fury. Anger often is confused with hostility, which is a habitual way of evaluating people or events in a negative, cynical, paranoid way. Most scientists believe the combination of hostility and unexpressed anger carries the greatest risk of heart disease.
- Cynicism represents mistrust of others and is usually the driving force behind hostility and predisposes to heart disease.
- Suspiciousness closely allies to cynicism. Being constantly on guard, making sure you always come out on top, and not trusting anyone results in over production of stress-producing hormones.
- The fifth and last coronary disease toxic trait is excessive self-involvement and false pride. This is the narcissist, the me-myself-and-I person, who always thinks of himself or herself first and foremost. Research suggests it is such excessive self-involvement that may be what actually causes hostility and anger, which so strongly link to heart disease.
Temperament traits and inflammation
The etiology and pathogenesis of cardiovascular (heart) disease is now considered to result from a chronic inflammatory process. In fact, the latest research suggests stress-induced inflammatory events may account for up to 40 percent of heart disease patients with no other known risk factors. Stress activates different body systems that cause release of various stress hormones like catecholamines, corticosteroids, glucagon, growth hormone, renin, and elevated levels of homocysteine. These substances induce a heightened state of cardiovascular activity, injured endothelium, and induction of adhesion molecules on endothelial cells to which recruited inflammatory cells adhere and translocate to the arterial wall.
 Inflammation is partly regulated by the steroid hormone cortisol secreted from the adrenal glands. Normally, cortisol functions to reduce inflammation, which is good. But over time, these efforts to reduce inflammation also suppress the immune system. Elevated stress, as observed in most Type A persons, initiates persistent and inconsistent elevations of blood cortisol. This results in a decrease in tissue sensitivity to cortisol. Specifically, immune cells become insensitive to cortisol’s regulatory effect. This promotes runaway inflammation that persists over time — a condition known as chronic inflammation.
Inflammation is partly regulated by the steroid hormone cortisol secreted from the adrenal glands. Normally, cortisol functions to reduce inflammation, which is good. But over time, these efforts to reduce inflammation also suppress the immune system. Elevated stress, as observed in most Type A persons, initiates persistent and inconsistent elevations of blood cortisol. This results in a decrease in tissue sensitivity to cortisol. Specifically, immune cells become insensitive to cortisol’s regulatory effect. This promotes runaway inflammation that persists over time — a condition known as chronic inflammation.
Recently, scientists from Stanford University linked 25 new genetic regions to coronary artery disease. They found that people with coronary artery disease are most likely predisposed to the disease because they have gene variants linked to inflammation — a genetic predisposition, perhaps caused in part by a certain temperament. A genetic predisposition coupled with the hurry-up disposition precipitates chronic inflammatory conditions, including atherosclerosis, some cancers, rheumatoid arthritis, periodontitis, asthma, chronic peptic ulcer, ulcerative colitis, Crohn’s disease, chronic sinusitis, chronic active hepatitis, Alzheimer’s disease, and even diabetes.
In other words, the inflammatory response is contained within the stress response and apparently associates with certain personality traits; i.e. the toxic core traits of the Type A personality. Apparently, during stress-induced anxiety, depression, or other psychosocial events, the body loses its ability to regulate the inflammatory response — and it proceeds unabated promoting the development and progression of disease.
Deterioration of coronary arteries
The accompanying figure shows progressive arterial blockage from a buildup of calcified fatty substances that progressively narrow an inflicted artery until it becomes totally closed-off; this is the disease of atherosclerosis. This disease is now known to be caused by chronic inflammation.
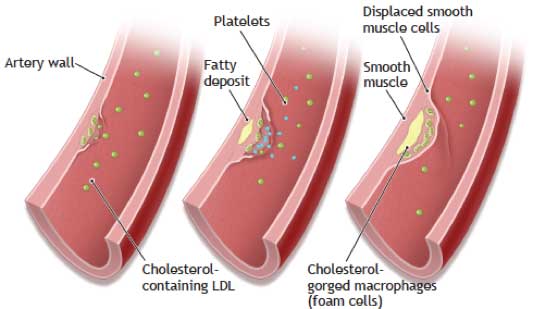 The first overt sign of atherosclerotic change occurs when lipid-rich macrophage cells (cells that engulf and digest debris and invading microorganisms) cluster under cells’ endothelial lining to form a bulge (fatty streak) in the artery. This is the first result of the inflammatory process.
The first overt sign of atherosclerotic change occurs when lipid-rich macrophage cells (cells that engulf and digest debris and invading microorganisms) cluster under cells’ endothelial lining to form a bulge (fatty streak) in the artery. This is the first result of the inflammatory process.
Over time, proliferating smooth muscle cells accumulate to narrow the artery’s opening. Typically a thrombus (or clot) forms that plugs the artery, depriving the heart muscle of normal blood flow and oxygen supply. When the thrombus blocks one of the smaller coronary vessels, a portion of the heart muscle dies (called necrosis), and the person experiences a myocardial infarction, commonly known as a heart attack.
If coronary artery narrowing leads to brief periods of inadequate blood flow, the person may experience intermittent pains known as angina pectoris. These pains usually emerge during exertion because there is a greater demand for blood flow in the heart muscle. Often, an angina attack provides the first painful, dramatic evidence of advanced inflammation-induced heart disease.
Tests of chronic inflammation
Unlike acute inflammation where you can feel, see, and overtly experience the process, the signs and symptoms of chronic inflammation are not so noticeable until the situation reaches a “clinical horizon.” That’s when overt symptoms appear. Often, these symptoms appear all of a sudden. More than half the individuals with pending coronary heart disease experience the first sign of serious inflammation during a heart attack or stroke.
There is no definitive test for chronic inflammation. The most trusted marker is measurement of blood levels of C-reactive protein (CRP) or an erythrocyte sedimentation rate (ESR) test.
CRP is an acute phase reactant, a protein made by the liver and released into the blood within a few hours after tissue injury, the start of an infection, or other cause of inflammation. The CRP test is not diagnostic of any one condition, but it can be used together with signs, symptoms, and other tests to evaluate an individual for an acute or chronic inflammatory condition. In most people CRP is low, usually below 1.0 mg/liter blood. If CRP is between 1.0 and 3.0, inflammatory risk is considered average. Risk is deemed high when CRP exceeds 3.0.
The erythrocyte sedimentation rate (ESR or sed rate) is another relatively simple, inexpensive, nonspecific test to help detect inflammation associated with inflammatory conditions such as infections, cancers, and autoimmune diseases. Blood is drawn and placed in a tall, thin tube. The red blood cells (erythrocytes) in whole blood gradually settle to the bottom. Inflammation causes cells to clump together. Because these clumps of cells are denser than individual cells, they settle to the bottom more quickly.
The sed rate test measures the distance red blood cells fall in a test tube in one hour. The farther the red blood cells have descended, the greater the inflammatory response of your immune system. Results are reported in the distance in millimeters red blood cells have descended in one hour. The normal range is 0-22 mm/hour for men and 0-29 mm/hour for women. The upper threshold for a normal sed rate value may vary somewhat from one medical practice to another, but in general values greater than 25 for men and 30 for women suggest inflammation.
References
- Assimes, T., 2015. “A comprehensive 1000 genomes-based genome-wide association meta-analysis of coronary artery disease.” Nature Genetics, Sept. 7. doi: 10.1038/ng.3396. [Epub ahead of print].
- Black, P.H., Garbutt, L.D., 2002. “Stress, inflammation, and cardiovascular disease.” Journal of Psychosomatic Research, 52(1):1-23.
- Eysenck, H.J., 1988. “Personality, stress, and cancer: Prediction and prophylaxis.” British Journal of Medical Psychology, 61:1, 57-75.
- Friedman, M., et al., 1986. “Alteration of Type A behavior and its effect on cardiac recurrences in post myocardial infarction patients: Summary results of the recurrent coronary prevention project.” American Heart Journal, 112 (4): 653–665.
- Friedman, M., 1996. “Type A behavior: Its diagnosis and treatment.” New York, Plenum Press (Kluwer Academic Press).
- Friedman, M. and Rosenman, R., 1959. “Association of specific overt behavior pattern with blood and cardiovascular findings.” The Journal of the American Medical Association, 169: 1286–1296.
- Sheldon, Cohen, et al., 2012. “Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk.” Proceedings of the National Academy of Sciences, DOI: 10.1073/pnas.1118355109.




Dr. John A. Romas, MPH, PhD - Rack ham Graduate School- Education & Public Health
I am a PhD graduate of U-M 1976. Implemented Public Act 226 on Family Planning and Reproductive Health, Administered Swine Flu Immunization & Efucation Program, and was State Health Consultant for the MI Department of Education. Taught at Wayne State University and U-M Extended Degree Program in Dearbirn. Prof EJ McClendon was my advisor at U-M- a great mentor!
I have nothing but admiration and praise from the schooling and education I received at U-M. Nothing less than quality! The article written above is another excellent piece of work on Stress and Health- the very nature of my professional career!
Sincerely,
JR
Reply