Spoiler alert

In hemodialysis, blood runs through a filter outside your body. With peritoneal dialysis, blood is cleaned inside your body.
I am one of the “every three adult Americans age 65 and older” who have chronic kidney disease (CKD). The condition is defined as a gradual and usually permanent loss of kidney function over months to years. I am successfully managing the condition with plant-based eating, physical activity, and other lifestyle modifications. I am writing this so others can be better informed and take action to “health themselves.”
Not necessarily a fait accompli
Most CKD patients do not progress to end-stage renal disease (ESRD) because they often die due to complications of coronary heart disease. Those who do reach end-stage renal disease may require renal replacement therapy (RRT), including hemodialysis, peritoneal dialysis, or kidney transplantation.
African Americans, Hispanics, Pacific Islanders, Native Americans, and the elderly face the highest risk for CKD development. Disturbingly, most individuals lack information about CKD and its symptoms and do not seek medical evaluation and care, even when a CKD diagnosis is confirmed.
Progression of kidney disease to dialysis, kidney transplant, or death need not be a fait accompli. Research suggests that when diagnosed early, and with careful attention to lifestyle changes, CKD can be controlled. I am banking on it!
How kidneys work
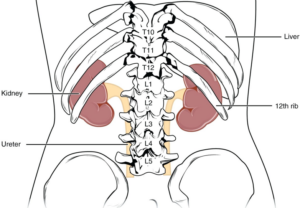 The kidneys are a pair of bean-shaped organs that lie on either side of the spine in the lower middle of the back. Each kidney weighs about 5 oz. and contains approximately one million filtering units called nephrons. Each nephron consists of a miniature filtering or sieving device called a glomerulus and a tiny tube-like structure, called a tubule, attached to the glomerulus.
The kidneys are a pair of bean-shaped organs that lie on either side of the spine in the lower middle of the back. Each kidney weighs about 5 oz. and contains approximately one million filtering units called nephrons. Each nephron consists of a miniature filtering or sieving device called a glomerulus and a tiny tube-like structure, called a tubule, attached to the glomerulus.
Kidneys perform many important functions, including:
 Ensuring there’s not too much or too little water in the body.
Ensuring there’s not too much or too little water in the body.- Removing waste products generated from normal metabolic processes, including breakdown of active tissues, ingested foods, and substances like urea, uric acid, and other wastes via urine.
- Being the active production site of biologically active vitamin D2 (calcitriol or 1,25 dihydroxy-vitamin D). D2 regulates the absorption of calcium and phosphorus from foods. It also promotes strong bone formation and production of erythropoietin, which stimulates bone marrow to produce red blood cells, and renin, which regulates blood volume and most importantly blood pressure in association with the hormone aldosterone. Aldosterone is manufactured in the adrenal glands just above the kidneys.
- Ensuring the body isn’t too acidic or too alkaline.
- Maintaining a balance of electrolytes like potassium, sodium, and calcium, important for maintaining heart rhythm.
The kidneys are connected to the urinary bladder by tubes called ureters. Urine is stored in the urinary bladder until the bladder is emptied by urinating. The bladder is connected to the outside of the body by another tube-like structure called the urethra.
Stages of CKD
CKD is diagnosed by the rate at which the kidneys’ glomerulus are able to filter blood, removing excess wastes and fluids. The glomerular filtration rate (GFR) is a calculation to measure kidney function. GFR is also one of the indices that defines different stages of CKD. The lower the GFR number, the worse the kidney function. Albumin represents the most common protein analyzed to check for signs of kidney disease. (Excess albumin in urine is termed albuminuria.)
High levels of albumin and low GFR values indicate different stages of CKD. The chart below illustrates the different stages of CKD, in this case using albumin and the GFR as indicators.
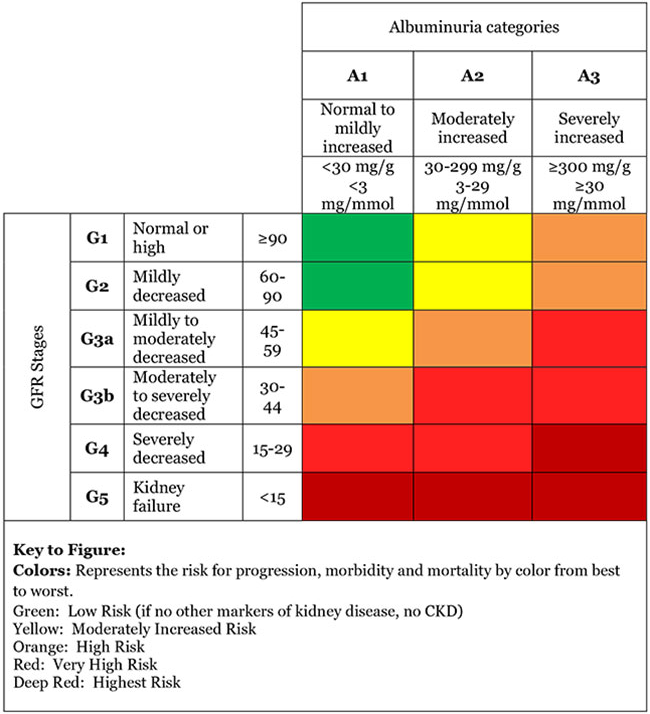
Generally, adults with normal kidney function have GFR numbers above 90. Having a GFR between 60-89 may be normal for some people, including those over age 60 since the GFR tends to decline with age, even in people without kidney disease. A GFR below 60 for three months or more suggests CKD.
CKD causes
The following factors predispose to CKD:
- Diabetes
- High blood pressure
- Heart disease
- Family member with CKD
- Being African American, Hispanic, Native American, or Asian
- Being older than age 60
CKD symptoms
CKD progresses slowly and symptoms may not appear until one is badly compromised. As CKD progresses one or more of the following symptoms can appear:
- Itching
- Muscle cramps
- Nausea and vomiting
- Diminished hunger
- Feet and ankle swelling
- Excess or diminished urine output
- Shortness of breath
- Sleep problems
If the kidneys stop working suddenly, termed acute kidney failure, one or more of the following symptoms can occur:
- Abdominal pain
- Back pain
- Diarrhea
- Fever
- Nosebleeds
- Rash
- Vomiting
If you have CKD
There are numerous steps that can slow CKD progression and protect the kidneys from further damage. The first step is to lower blood pressure to below 130/80 mmHg. The most cost-effective, non-pharmacological approaches to lowering blood pressure include modifying diet (see below), increasing physical activity, decreasing excess body weight, decreasing stress, improving sleep quality, lowering blood glucose (if diabetes or prediabetes are present), and smoking cessation.
Diet intervention and CKD
Specific dietary interventions can potentially decrease incidences of CKD. This has been an understudied topic until recently. But one large-scale study, published in 2015, examined 15,055 middle-aged, community-dwelling adults (with a mean age of 54). Researchers assessed participants’ dietary intakes at baseline (1986-89) and again later (1993-95).
During follow-up, the researchers identified 2,351 individuals with stage III-CKD. They identified individuals who also had an accompanied >25 percent decline in GFR from baseline. This study revealed individuals with CKD experienced lower disease progression when they consumed more plant proteins compared to more animal proteins. These results confirm data from other smaller studies showing plant-based diets associate with decreased mortality from CKD and related causes.Since diabetes and hypertension are the leading causes of CKD, it makes sense that dietary patterns known to decrease incidence of these two conditions could also reduce CKD progression. Ample evidence now exists that plant-based diets, low in salt and high in nuts, unsaturated fats, seeds, whole grains, fruits, and vegetables decrease incidence of type 2 diabetes, lower blood pressure, and decrease risk of heart disease.
Not surprisingly, the National Kidney Foundation also says CKD patients may benefit from vegetarianism or a part-time vegetarian diet.
 Experts may debate the effects of plant-based diets on CKD progression. But it cannot be denied that a plant-based diet does have favorable effects on the most deleterious cardiovascular and metabolic disorders associated with CKD, such as hypertension and diabetes. This makes for a sound and defensible rationale for recommending a plant-based diet for patients with failing kidneys.
Experts may debate the effects of plant-based diets on CKD progression. But it cannot be denied that a plant-based diet does have favorable effects on the most deleterious cardiovascular and metabolic disorders associated with CKD, such as hypertension and diabetes. This makes for a sound and defensible rationale for recommending a plant-based diet for patients with failing kidneys.
Two potential drawbacks of plant-based diets are the amount of phosphorus and potassium found in plant foods, which can stress ailing kidneys. But it turns out that the phosphorus in meat is absorbed at about twice the rate of plant-based phosphorus, not to mention the phosphate additives that are injected into different meats. So, eating vegan-vegetarian can significantly lower phosphorus levels in the blood. Potassium can create problems for patients on dialysis or with end-stage disease. People with reduced, but normally functioning kidneys, tend to be all right, however, since the alkalinizing effects of plant foods help the body excrete potassium.
Specific dietary recommendations
- Reduce or eliminate animal protein; eat a plant-based diet as much as possible
- Choose and prepare foods with less salt
- Buy and prepare fresh food as much as possible
- Try to avoid prepared foods, fast foods, frozen dinners, and canned foods that are high in salt, or “non-nutritional” phosphorus
- Use spices, herbs, and sodium-free seasonings in place of salt; avoid “salt substitutes” that are high in potassium
- Rinse canned foods with water
I have written about the benefits of a mostly plant-based diet in previous issues of Michigan Today: “Whole-food, plant-based nutrition,” “Food as medicine,” and “Food as medicine, part 2.” I hope these columns help you decide what is best for your body.
References
- Chen, X., Beddhu, S. 2015. “Food for thought: Diet as a risk factor for CKD.” American Journal of Nephrology; 42:425.
- Chen, X., et al. 2015. “The associations of plant protein intake with all-cause mortality in CKD.” The American Journal of Kidney Diseases; pii:S0272-6386(15)01339-6.
- Coresh, J., et. al. 2007. “Prevalence of chronic kidney disease in the United States. The Journal of the American Medical Association;298:2038.
- Gluba-Brzózka, A., et. al. 2017. “Vegetarian diet in chronic kidney disease: A friend or foe?” Nutrients; 9(4):374.
- Lin, J., et. al. 2011. “Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses’ Health Study.” The American Journal of Kidney Diseases; 57:245.
- National Institute of Diabetes and Digestive and Kidney Diseases
- Rahul, A., et. al. 2019. “Mortality outcomes with intensive blood pressure targets in chronic kidney disease patients: A pooled individual patient data analysis from randomized trials.” Hypertension; 73:1275.
- Rebholz, C., et al. 2015. “Dietary acid load and incident chronic kidney disease: Results from the ARIC study.” American Journal of Nephrology; 42:427.
- Smyth, A., et. al. 2016. “Diet and major renal outcomes: A prospective cohort study,” The NIH-AARP Diet and Health Study. Journal of Renal Nutrition; 26(5):288.
- Turin T.C., et. al. 2012. “Lifetime risk of ESRD.” Journal of the American Society of Nephrology; 23(9):1569.
- United States Renal Data System report captures the high burden, high cost and low awareness of kidney disease in the united states.
- The kidney failure risk equation: Find out your real risk of kidney failure.
- van der Velde, M., et. al. 2011. “Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts.” Kidney Internationa; 79:1341.


